Automated detection and classification of patient–ventilator asynchrony by means of machine learning and simulated data
Collecting the results of international fellows coming to Pavia from Eindhoven Technical University for research on respiratory patients: machine learning for detection and classification of patient-ventilator asynchronies.
Free full text here on Computer Methods and Programs in Biomedicine
Abstract
Background and objective
Mechanical ventilation is a lifesaving treatment for critically ill patients in an Intensive Care Unit (ICU) or during surgery. However, one potential harm of mechanical ventilation is related to patient–ventilator asynchrony (PVA). PVA can cause discomfort to the patient, damage to the lungs, and an increase in the length of stay in the ICU and on the ventilator. Therefore, automated detection algorithms are being developed to detect and classify PVAs, with the goal of optimizing mechanical ventilation. However, the development of these algorithms often requires large labeled datasets; these are generally difficult to obtain, as their collection and labeling is a time-consuming and labor-intensive task, which needs to be performed by clinical experts.
Methods
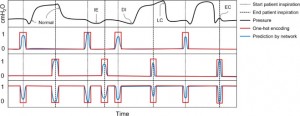
In this work, we aimed to develop a computer algorithm for the automatic detection and classification of PVA. The algorithm employs a neural network for the detection of the breath of the patient. The development of the algorithm was aided by simulations from a recently published model of the patient-ventilator interaction.
Results
The proposed method was effective, providing an algorithm with reliable detection and classification results of over 90% accuracy. Besides presenting a detection and classification algorithm for a variety of PVAs, here we show that using simulated data in combination with clinical data increases the variability in the training dataset, leading to a gain in performance and generalizability.
Conclusions
In the future, these algorithms can be utilized to gain a better understanding of the clinical impact of PVAs and help clinicians to better monitor their ventilation strategies.